Abstract
Background
Advances in hematopoietic cell transplantation (HCT) over the past decades have led to improvements in HCT outcomes. However, allogeneic HCT continues to be associated with significant morbidity and mortality, making end-of-life (EOL) planning and management especially important in this patient population. A paucity of data exists on the utilization of advance care planning (ACP) amongst allogeneic HCT recipients, and the relationship between ACP and intensity of EOL health care utilization in these patients.
Methods
We performed a retrospective review of patients receiving allogeneic HCT at our institution from 2008 to 2015 who had subsequently died following HCT. Frequency and timing of advance directive (AD) completion were abstracted from the electronic medical record (with local chart review when possible), as were patient demographics, HCT outcomes, intensive care unit (ICU) days, use of mechanical ventilation, and location of death. Variables associated with the utilization of AD were compared using Chi-square and Wilcoxon rank sum test. Multivariable logistic regression evaluated variables associated with EOL ICU utilization.
Results
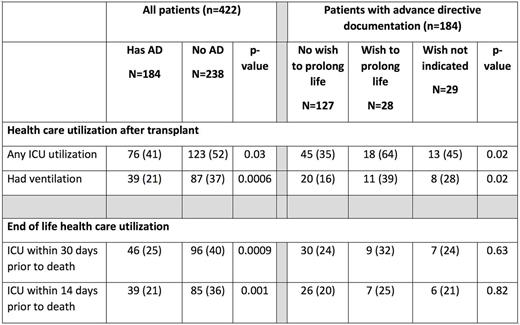
Of the 1031 patients who received allogeneic HCT during the study period, there were 422 (41%) decedents who are included in the analysis. Median age at time of transplant was 55 years (IQR, 44 to 64 years), 58% were male, and 56% were Non-Hispanic White. Acute myeloid leukemia (AML) was the most common primary disease (41%); 23% of the subjects died within 100 days of transplant date. 184 (44%) patients had an AD documented prior to death. Among patients with an AD, 105 (57%) completed the AD in the pre-transplantation period. A majority of patients (69%) indicated on the AD that if terminally ill, they did not wish to be subjected to life-prolonging treatment attempts. Race/ethnicity was significantly associated with AD documentation, with Non-Hispanic White patients documenting ADs more frequently (74%) compared to Hispanic (7%) or Asian patients (11); p= 0.0007. Patients with AD were less likely to utilize the ICU during the transplant course (41% for patients with AD versus 52% of patients without AD; p= 0.03) and also were less likely to receive mechanical ventilation at any point following transplantation (21% versus 37%; p<0.001). AD was also associated with decreased ICU utilization at the end-of-life; 25% versus 40% with and without AD were admitted to the ICU within 30 days of death (p<0.001), and 21% versus 36% with and without AD were admitted to ICU within 14 days of death (p=0.001). Amongst those with an AD, patients who indicated a wish for life-prolonging treatment attempts were significantly more likely to utilize the ICU (64% versus 35%; p=0.02) and were also more likely to have mechanical ventilation at any point after transplant (39% versus 16%; p=0.02). Compared to patients without AD, patients with AD were more likely to die at home or in hospital as opposed to in the ICU (p=0.03).
Conclusion:
Our results suggest that adoption of a systematic practice to standardize advance directive documentation as part of allogeneic HCT planning has the potential to significantly reduce ICU utilization and mechanical ventilation while improving quality of care at end-of-life in HCT recipients. Culturally sensitive approaches that focus on what matters most to the patient may help ethnic minority patients complete ACP.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal